Medicaid Check-In: Partnerships in Maryland to Keep our Community Covered
Collaborative Partnerships in Maryland
In March 2020, Congress passed a law prohibiting states from terminating any enrollee’s Medicaid coverage due to loss of eligibility during the COVID-19 Federal Public Health Emergency (PHE). That law was subsequently amended such that states will begin reviewing Medicaid eligibility in April 2023. The prohibition resulted in national Medicaid enrollment swelling to its largest-ever level (1.7 million enrollees in Maryland) and the uninsured rate dropping to its lowest.
Starting in April 2023, Maryland will resume eligibility reviews (redeterminations), which will take place over 12 months. To ensure continuity of coverage for those who remain eligible for Medicaid and those who do not, partnership and collaboration between and among federal and state governments, Medicaid Managed Care Organizations (MCOs), health insurance exchanges, providers, and community partners is necessary. Due to ongoing preparation during the pandemic, Maryland stands out as among the nation’s leaders in redetermination planning, recognizing the power of multi-stakeholder collaboration to preserve continuity of coverage for enrollees.
Medicaid Check-In Campaign Timeline
Pre-Launch – Awareness Update (Feb 28/March 2023 – April 1)
- Remind enrollees to update contact information.
Launch –Redetermination Action (April 15, 2023 – April/May 2024)
- Encourage enrollees to keep contact information current and educate enrollees on renewal process.
Medicaid Check-In Campaign Strategies
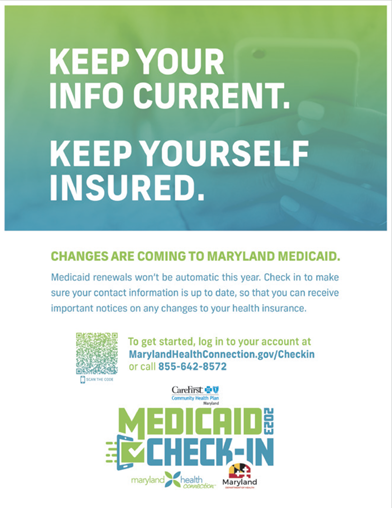
Maryland Department of Health (MDH) and the 9 MCOs have collectively invested $3 million in a statewide campaign to provide unified messaging to beneficiaries through the multi-modal “Medicaid Check-In” campaign to reach enrollees wherever they are. Statewide strategies include broad awareness and education via TV, radio, social media, and robocalls. MCO-driven strategies involve member communication via text messages, emails, direct mail, outreach events, and outbound calls.
For more information contact: Sarah Meek, Director of Federal Affairs at CareFirst BlueCross Blue Shield sarah.meek@carefirst.com.
- 24% of Marylanders are covered under Medicaid
- 47% of children under 18 are covered under Medicaid
- 46% of members are female
- As many as 80,000 MD Medicaid members could lose coverage during the redetermination period
- HealthChoice MCOs (Aetna Better Health, CareFirst BlueCross BlueShield Community Health Plan Maryland, Jai Medical Systems, Kaiser Permanente, Maryland Physicians Care, MedStar Family Choice, Priority Partners, UnitedHealthcare, Wellpoint Maryland)
- Maryland Department of Health
- Maryland Department of Human Services
- Maryland Health Connection
- Maryland Health Benefit Exchange
- GKV (Communications Firm)
- Chesapeake Regional Information System for our Patients (CRISP)
- Providers
- Community-based organizations
- Centers for Medicare & Medicaid Services (CMS)
Provider & Community Outreach
MDH and MCOs are working alongside local councils, community based organizations, and providers to promote awareness of Medicaid redeterminations. Examples include:
- Hosting Community Advisory Community meetings attended by 60+ organizations statewide, which have been instrumental in informing stakeholders of the upcoming change.
- Working with CVS to direct members to update information.
- Developing a Provider/Community Toolkit to support providers, advocates, and partners with key messaging and resources to make sure members know how to renew their coverage or obtain other affordable health coverage options if needed.
What You Can Do
Help ensure that Marylanders avoid disruptions in health care coverage by reminding enrollees to update their contact information in Maryland Health Connection. You can encourage enrollees to do the following:
- Check in with Maryland Health Connection to make sure contact information is up to date. Marylanders with Medicaid or CHIP coverage can update their contact information in three ways: online at MarylandHealthConnection. gov, by phone, or in person. For Marylanders who qualify for Medicaid because they are aged, blind, disabled, or enrolled in a Home and Community-Based Services Program, these individuals can update their contact information by visiting their local Department of Social Services, calling 800-332-6347, or visiting mymdthink.maryland.gov.
- Watch for communications from Maryland Health Connection. Different groups will be notified at different times and will have 45 days to respond.
- Renew coverage or enroll in a private plan when receiving their notice. Enrollees will receive a notice in the mail or in their online account. This notice will tell enrollees to complete their renewal or if they are no longer eligible for Medicaid coverage. If an individual is no longer eligible for Medicaid, they can enroll in a low-cost health insurance option, such as a private plan, through Maryland Health Connection within 60 days of losing health coverage. If enrollees fail to respond, their Medicaid coverage will end.
For More Information
Enrollees can get help online, in person or by phone:
- Call Maryland Health Connection at 855-642-8572. Help is available in more than 200 languages. Deaf and hard of hearing use can use relay service.
- Call or visit your local Department of Social Services.
- Call or visit your local Health Department.
- Connect with a broker or navigator.