COVID-19 Vaccine Information
About the Vaccines
To protect yourself and your loved ones, it’s important to get vaccinated. COVID-19 vaccines and boosters are now widely available.
What COVID-19 vaccines are currently available?
The Pfizer-BioNTech vaccine is available for individuals ages 6 months and older.
The Moderna vaccine/Spikevax COVID-19 vaccine is available for people 6 months and older.
The FDA has issued emergency use authorization (EUA) for the Novavax COVID-19 vaccine as another primary series for people 12 and older. Novavax’s COVID-19 vaccine is protein-based (rather than mRNA). This vaccine technology has been around in vaccines for decades in the U.S.
How much will the vaccine cost?
If you’re a current CareFirst member, you’ll pay $0 for any FDA authorized vaccine.
Were different races and ethnicities included in the original/initial vaccine trials?
Yes. For details, see the charts below.
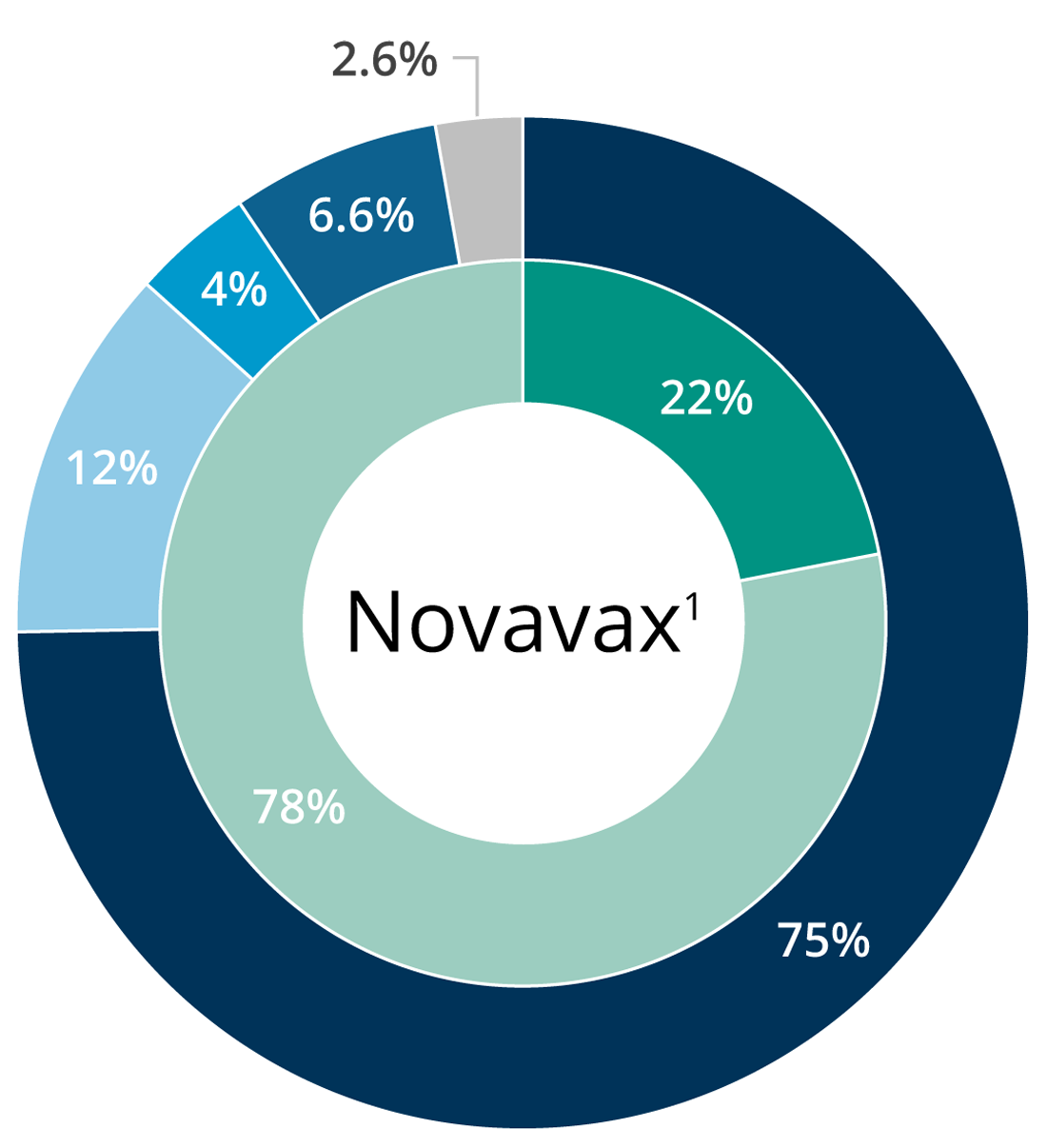
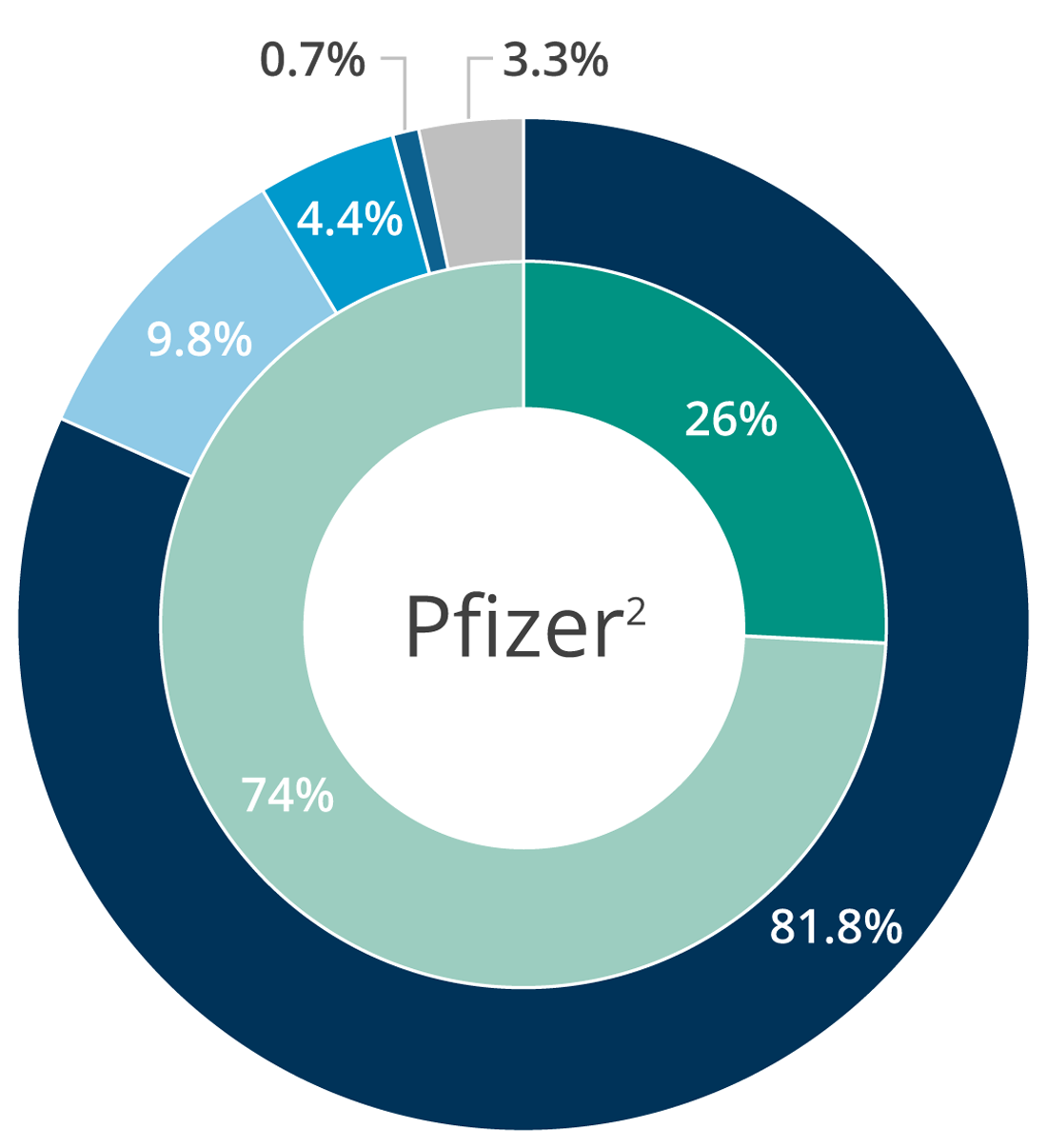
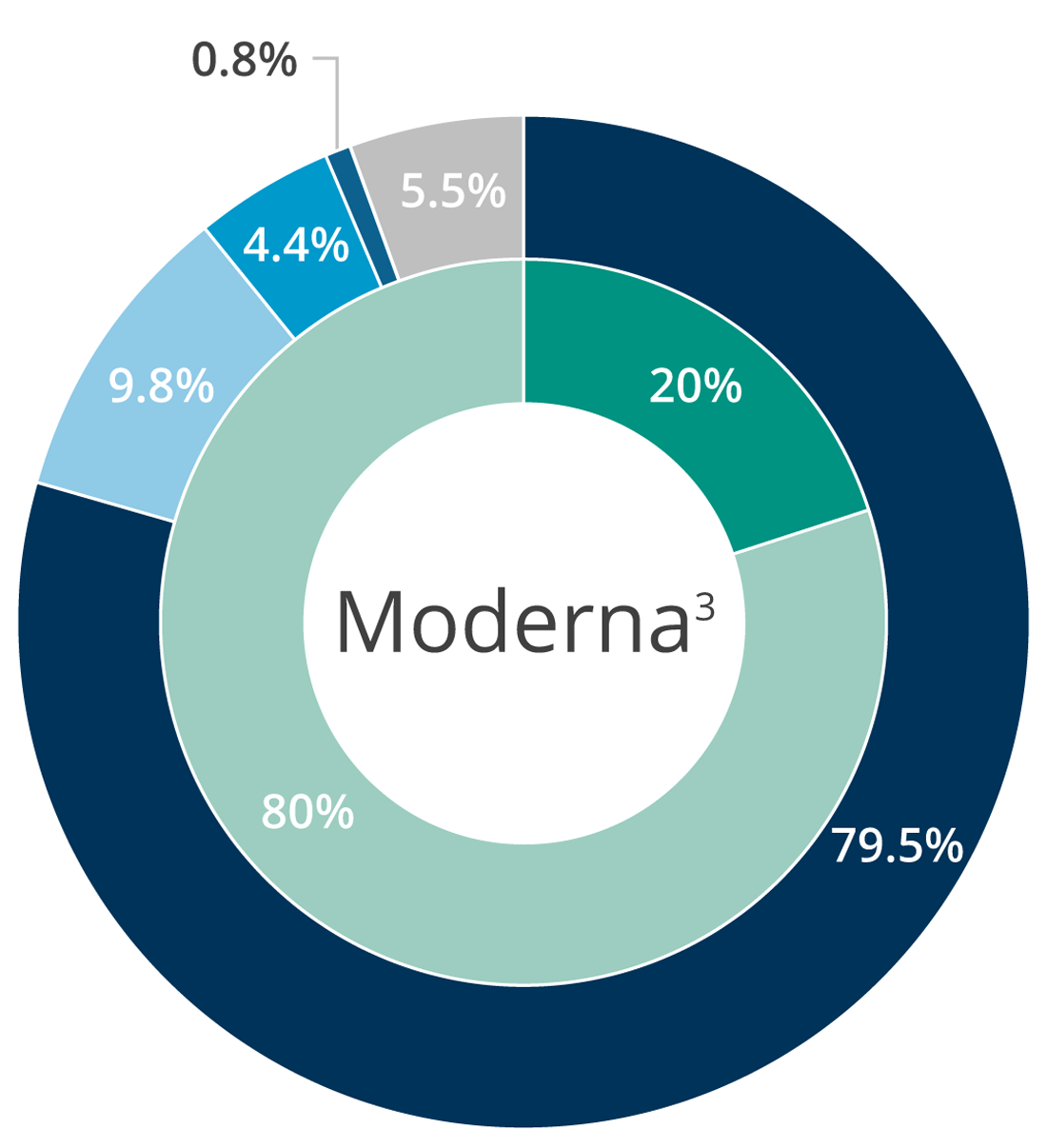
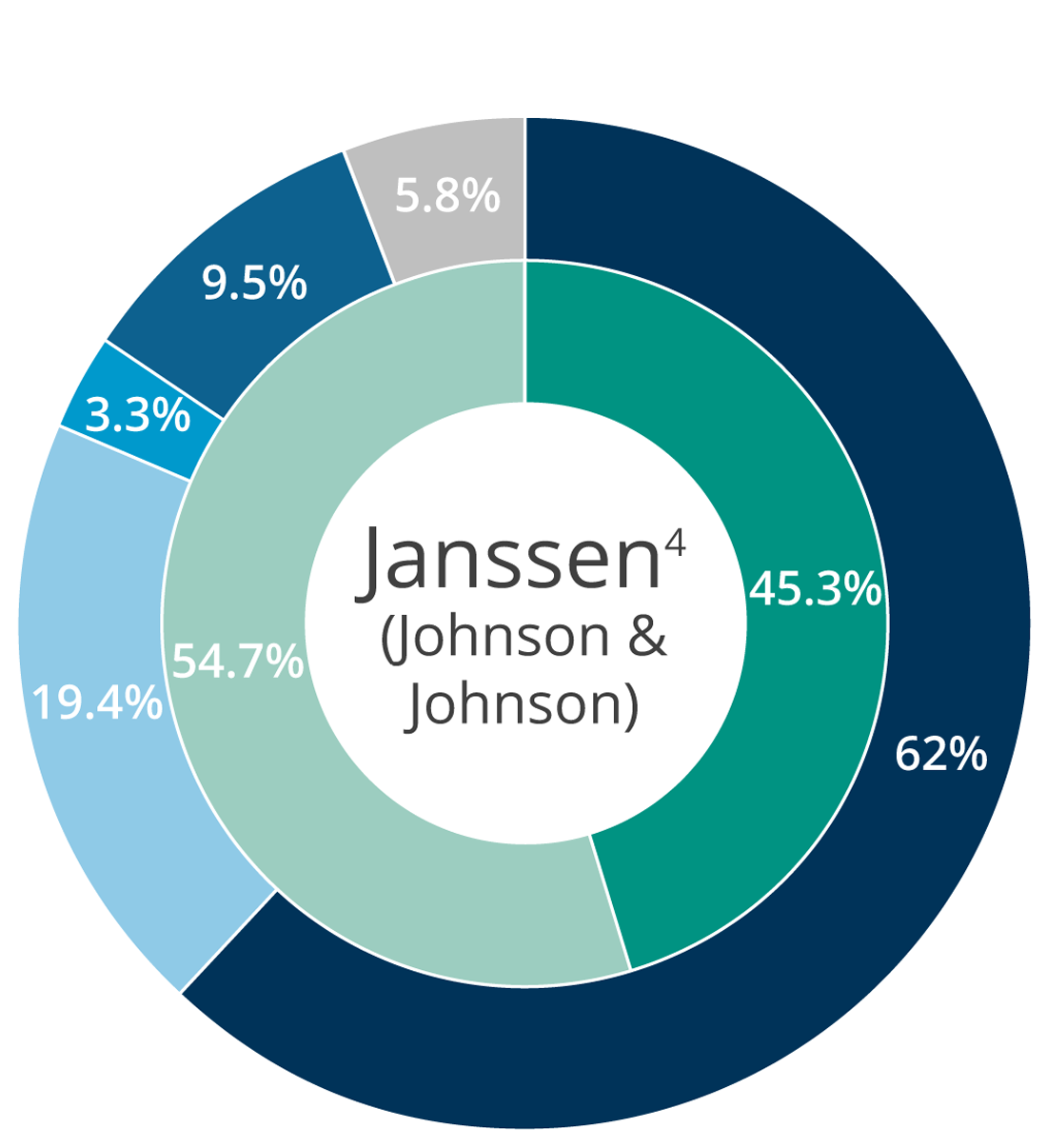

*Percentages add up to more than 100% when study participants self-identify in two categories.
- Centers for Disease Control and Prevention. FDA Briefing Document Novavax COVID-19 Vaccine, June 2022. https://www.fda.gov/media/158912/download. September 2022.
- Centers for Disease Control and Prevention. FDA Briefing Document: Pfizer-BioNTech COVID-19 Vaccine, December 2020. https://www.fda.gov/media/144245/download. September 2022.
- Centers for Disease Control and Prevention. FDA Briefing Document Moderna COVID-19 Vaccine, December 2020. https://www.fda.gov/media/144434/download. September 2022.
- U.S. Food & Drug Administration. Janssen COVID-19 Vaccine Frequently Asked Questions. https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-frequently-asked-questions. September 13 2022.
| Ethnicity | Percentage |
|---|---|
| White | 57% |
| Hispanic / Latinx | 26% |
| Black | 10% |
| Asian | 4% |
| Other racial groups | 3% |
| Ethnicity | Percentage |
|---|---|
| White | 63% |
| Hispanic / Latinx | 20% |
| Black | 10% |
| Asian | 4% |
| Other racial groups | <3% |
| Ethnicity | Percentage |
|---|---|
| White | 63% |
| Hispanic / Latinx | 20% |
| Black | 10% |
| Asian | 4% |
| Other racial groups | <3% |
| Ethnicity | Percentage |
|---|---|
| White | 17% |
| Hispanic / Latinx | 45% |
| Black | 19% |
| Asian | 3% |
| American Indian/Alaska Native | 10% |
| Other racial groups | <6% |
How should I prepare myself and my body for the COVID-19 vaccine?
Preparing for your COVID-19 vaccination is pretty straightforward. Be sure to get a good night’s rest before your appointment and try to show up as hydrated as possible. Before you go, be sure to discuss any medical concerns with your doctor.
It’s currently recommended that you avoid taking over-the-counter pain medicine before you receive your vaccination, like ibuprofen, aspirin and acetaminophen, unless you take these regularly for other reasons. If needed, you may take over-the-counter pain relievers after your shot. It’s also recommended that you avoid taking antihistamines, like Loratadine and Cetirizine. These may help with seasonal or other allergies, but they won’t prevent any vaccine-related allergic reactions. Find out more about preparing for your COVID-19 vaccination from the CDC.
Can you still catch COVID-19 after being vaccinated?
All authorized COVID-19 vaccines are extremely effective, but no vaccine or medical treatment is 100% effective. Plus, the vaccination process takes time. You aren’t fully protected until two weeks after your last vaccine dose.
Another reason you could test positive after vaccination is that COVID-19 has a 2–14-day incubation period. It’s possible that you were infected with COVID-19 before you got your vaccine, but you didn’t experience symptoms until a few days later. Remember, even if the vaccine doesn’t prevent you from catching COVID-19, it will lessen the severity of the infection and significantly reduces the chance of hospitalization.
What should I do if I can’t or don’t want to get vaccinated?
To reduce the spread of the disease, and to avoid catching COVID-19, continue to follow existing safety guidance:
- Wear a mask when you’re around other people.
- Wash your hands regularly.
- Get a flu shot—flu shots can protect you from other types of serious illness that may require hospitalization. Visit our CareFirst vaccine information page to see where you can get your flu vaccine this season—it’s more important than ever.
Why do the COVID-19 vaccines have to be stored in such cold temperatures?
The Pfizer and Moderna vaccines are what’s known as mRNA vaccines. They contain many enzymes which can easily break the vaccine apart and destroy it in warmer temperatures. The extreme cold slows this process down significantly, which keeps the vaccines stable and “fresh” longer.